Gestational Diabetes
Bummer News
It sucks to receive the result that you didn’t pass the glucose tolerance test. You might be feeling like it’s your fault and you “failed”, worried about your baby’s health, jealous of all the other pregnant people who get to indulge their cravings carefree, etc.
This is all understandable; a few points to keep in mind that may soften the blow:
While some women get diabetes because they eat poorly, there is a portion of women who will get it because of genetics and insulin resistant hormones pumped out by their placenta. If you do not fit the typical high-risk category, it’s likely that you are just unlucky, so try to release any blame you’ve put on yourself.
They do the glucose test at this stage in pregnancy for a reason - you haven’t done any harm to your baby, and going forward you can minimize any negative impact through managing it with diet, exercise, and (if necessary) insulin
One silver lining is that you will likely be in much better shape by the time you give birth, and have an easier time getting back to pre-pregnancy weight after birth
What now?
Your OB will likely connect you with a nutritionist who will check in at regular intervals
You will get a prescription for a glucometer to start tracking your blood sugar; this involves pricking your finger 4 times a day: when you wake up (“fasting blood sugar”), and 1 hour after breakfast, lunch and dinner. It’s not that painful and you’ll end up getting used to it - pricking the side of your finger hurts less than pricking directly underneath.
CGMs (continuous glucose monitors) that go in your arm are less accurate than finger pricks, especially during pregnancy because they rely on measuring glucose in interstitial fluid rather than blood directly, and fluid retention is way higher during pregnancy which can mess with the data
However, if you’d like to use a CGM in addition to the blood glucometer, it can be useful to observe trends throughout the day, just don’t put too much stock in a single-point-in-time reading - Stelo by Dexcom is recommended, but you’ll have to pay for it yourself (~$100/month)
You will start using the dual levers of diet and exercise to keep your blood sugar within a safe range. This will get harder as you progress through your pregnancy and insulin resistance rises, so you may eventually need to also utilize insulin injections (about 15% of women with GD end up needing insulin) or an alternative oral medication called glyburide. Again, this is based on your hormones and not a reflection of how “well” you are doing with diet/exercise.
I needed to go on nightly insulin with my third pregnancy to control fasting levels, and while I was initially very resistant to the idea, the injections ended up not being a big deal and actually took some of the stress away
With insulin, you can expect more frequent appointments to monitor your baby, including regular non-stress tests (measuring amniotic fluid levels and baby’s heart rate patterns)
Start tracking your blood sugars - I’ve created two different Excel trackers here, one that just includes blood sugars, and one that also notes food and exercise so you can see any patterns. Make a copy of this doc so you can edit with your own data. It’s okay if you don’t remember to test or track every single time, it’s the general trend that matters.
There’s also a new GD tracking app called Malama or you can keep it simple and just use the “Notes” app on your phone
Try your best to stay within the ranges as much as possible, but don’t beat yourself up over an occasional bad reading. Fasting BS can be especially hard to influence since it’s affected by what your body does overnight which is less in your control. Your doctor will give you specific guidelines about how many high readings are concerning, but generally you’d want to reach out to your team if you’re having over 3 readings a week above the targets.
You will likely have at least one additional ultrasound to ensure that the baby is not growing too large - that is the main risk of GD, that too much sugar gets to the baby. It’s nice to get to say hi to your baby one extra time!
You will have some additional monitoring during labor to check that blood sugar levels are in range. Once baby is born, baby will also have a couple extra tests (heel pricks) to test blood sugar, because they may struggle with insulin regulation due to the GD.
The majority of people with gestational diabetes will return to normal after giving birth - you’ll get tested 6-12 weeks after delivery, and every couple years. And around half of women will have GD again in subsequent pregnancies.
My Top 10 Tips
Pair your Carbs with Fat/Protein: You can still eat carbs, you just need to be more strategic - the best thing you can do is always “dress” your carbs with fat or protein, to help reduce the glucose spike. This looks like adding avocado to toast, peanut butter with apples, cheese with crackers, etc. The IG account glucosegoddess has great tips and graphics to illustrate this:
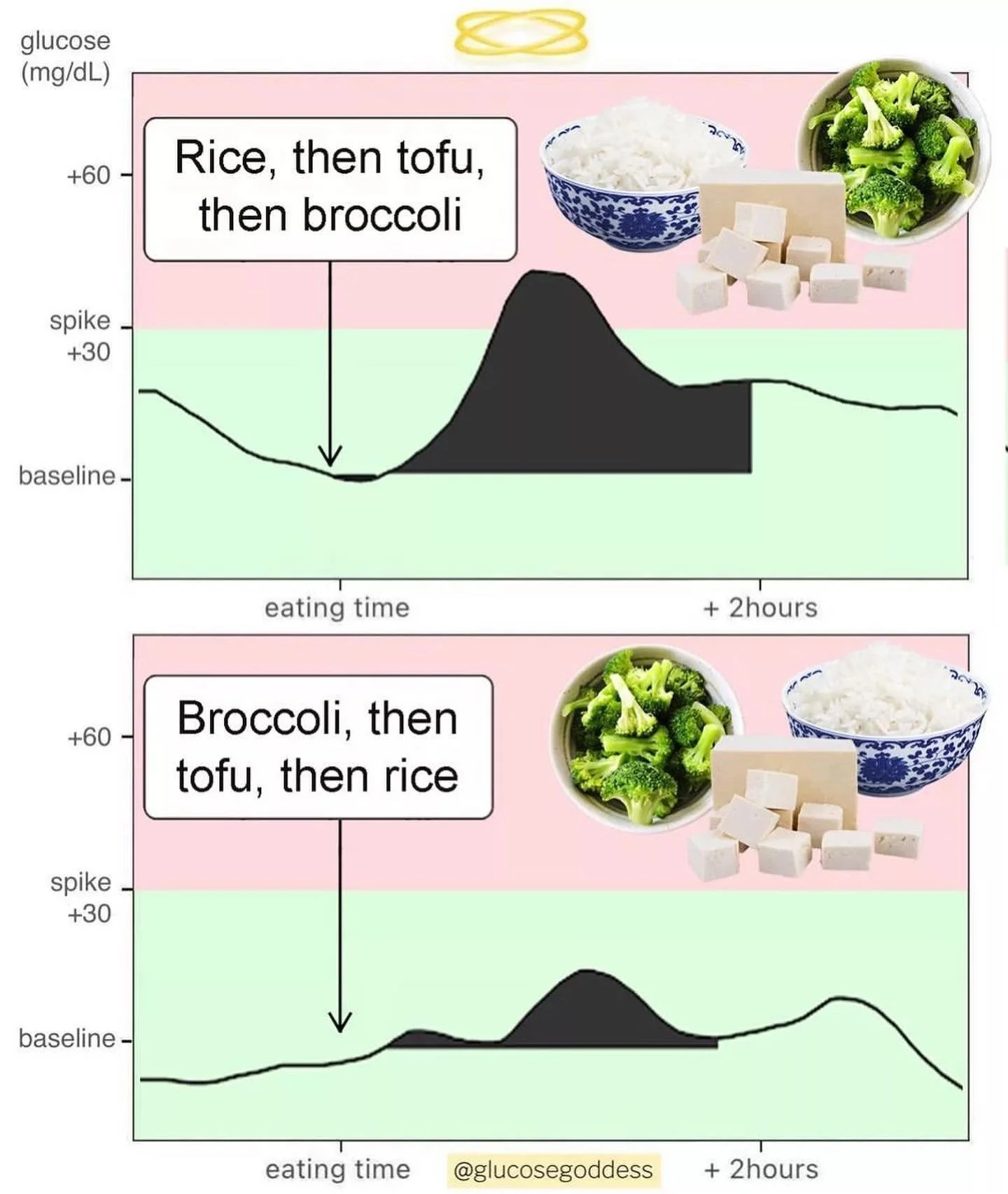
2. Order Matters: if you’re going to have carbs during a meal, it’s better for your glucose levels to have them after having veggies or protein. So resist the bread rolls at the restaurant until after you’ve had your salad course, for example. Also, if you’re going to indulge in a sweet, have it as dessert after a meal rather than separately on an empty stomach (and ice cream is a much better dessert choice than cookies/cake because it has protein/fat in addition to sugar).
3. Not all Carbs are Created Equal: fiber is much better for blood sugar than starches or sugars, so prioritize carbs like chickpeas/lentils, oatmeal, non-starchy veggies, and look up whether a given fruit has a low or high glycemic index. More hacks: fresh fruit is better than dried fruit; sourdough bread is better than white.
4. Smaller, more frequent meals: this keeps your blood sugar more stable by ensuring you’re never having too much carbs at a given time, while still making sure you’re getting adequate nutrition and calories for your baby. I recommend a morning, afternoon and evening snack, aiming to eat every 2-3 hours. If you are too restrictive on calories/carbs, it may actually backfire and your body might compensate by releasing more glucose at night, raising your morning fasting levels.
5. Explore New Brands: given the popularity of low-carb diets like Keto, it’s actually a much better time to have GD because there are lots of creative brands out there:
Fairlife or Koia shakes: these high protein, low sugar shakes are easy to grab when you don’t have time and taste surprisingly good - I like the Chocolate/Cacao Bean flavor most
Edamame Pasta: high protein, tastes good with pesto; fettuccine or spaghetti
Banza: chickpea based pasta (comes in many different pasta forms) - still fairly high carb, but at least balanced out by protein
Yasso Bars: greek-yogurt based ice cream bars
Keto Cups: low sugar nut-butter cups
Lily’s Chocolate: sweetened with stevia, which doesn’t affect blood sugar
Tessamae’s Salad Dressing: sugar-free
6. Takeout is Tricky: when you’re cooking food yourself, you’re aware of the ingredients, but with takeout or restaurant food, there may be a surprising amount of sugar hidden in things like sauces. I’m not saying to avoid restaurants all together - you still gotta live your life - but try to do extra exercise after those meals, or only indulge in a BS spiking dish if it’s really delicious and worth it (e.g. a bowl of pasta at your favorite amazing restaurant vs. at a dumpy place where quality is unknown).
7. Build Exercise into your Schedule: Does your commute to work involve a walk? If so, try to eat breakfast before you leave so that you can walk it off. Add a recurring calendar block after lunch at work so that you can get some exercise, or if you have a recurring meeting see if it’s possible to make it a walking meeting. If you have a standing desk, try to stand after a meal since that will burn more calories. And involve your partner or friends in making it a ritual to do a post dinner walk together.
8. Any Exercise Counts: don’t let the perfect be the enemy of the good! Even doing dishes and other chores after dinner is still more movement than laying on the couch. While it’s most effective to exercise after a meal, it is still beneficial if you exercise before if that’s more convenient. I enjoyed doing lunges and squats around the dinner table, and my dinner-mates found it entertaining. Interestingly, exercising too hard (like an intense Peloton intervals ride) can actually raise your blood sugar, so opt for lower intensity cardio like walking or moderate cycling.
9. Hydrate: pretty simple - drinking water lowers the concentration of glucose in your blood. Staying hydrated is already important during pregnancy, so here’s yet another reason.
10. Consider other factors affecting blood sugar: you may notice your blood sugar levels increase after a bad night of sleep, or if you are fighting a sickness. This is normal, so don’t worry that it’s something you’ve done wrong on the diet/exercise front.
Finally, remember: this is temporary and for the good of your baby!